Apgar scale for assessing the health status of a newborn baby. Grades - from birth. What is the Apgar score? Apgar scale 8 9 points interpretation ep
The Apgar score after 1 minute indicates the initial condition of the newborn and indicates those children who require more attention, and the score at 5 minutes indicates effectiveness. Therefore, there are always two Apgar scores, for example 8/8 points. In most newborns, the condition 1 minute after birth on the Apgar scale is estimated at 7-8 points; after 5 minutes, the general condition of these newborns corresponds to 8-10 points, which is prognostically favorable. If a mother finds out that her baby has been diagnosed 8 points, then gets very upset.
The first test that newborns undergo (and most do well) is the Apgar score. The test was proposed in 1952 by American anesthesiologist Virginia Apgar. The result, recorded one minute after birth and recorded again 5 minutes later, reflects the overall condition of the newborn and is based on observations in five assessment categories. Children who score between 7 and 10 are considered good or excellent and usually require only routine care; those who score between 4 and 6 points are in fair condition and may only require some resuscitation procedures; and those whose score is less than 4 require immediate assistance to save their life. At one time it was believed that children whose score remained low 5 minutes after birth were doomed to have neurological problems in the future, but recent studies have shown that most of these children grow up normal and quite healthy.
Apgar score.
To identify hypoxia and determine its degree, newborn children are usually assessed using the Apgar scale (see table below). The assessment is carried out at 1-5 minutes of life using 5 clinical signs, each of which is scored from 0 to 2 points. The maximum amount is 10, the minimum is 0. A score from 1 to 4 points indicates severe hypoxia, and 5-6 indicates mild hypoxia. A score from 7 to 10 indicates a satisfactory condition.
It should be emphasized that the Apgar score unilaterally characterizes the condition of newborns. It states the presence or absence of hypoxia at the time of birth. If low scores on the Apgar scale guide the doctor towards antihypoxic therapy, including resuscitation, then a score of 7-9 points does not guarantee complete well-being. A few hours after birth, the condition may deteriorate due to respiratory distress syndrome or other pathology.
Apgar score table
Assessment of the condition of a newborn baby in the first minute of life
| Signs | 0 points | 1 point | 2 points |
| Pulse | Absent | Less than 100 beats/min | More than 100 beats/min |
| Breath | Absent | Slow, irregular | Good, shout |
| Muscle tone | Weak | Bends arms and legs | Actively moving |
| Reflexes (reaction to a catheter in the nose) | Absent | Grimaces | Sneezes, coughs, pushes away |
| Color of the skin | Blue, pale | Normal, but bluish arms and legs | Normal throughout the body |
Evaluation of Apgar test results
This testing is usually carried out within one to five minutes after the baby is born, and can be repeated later if the results are poor.
Scores less than 3 indicate a critical condition of the newborn, more than 7 is considered a good condition (normal).
The Apgar score was developed for health care providers to determine which children require closer monitoring.
The child who received 5 points, needs closer monitoring than a child who has received 7-10 points.
A child who received a scale 5-6 points a minute after birth, but five minutes later it increased to 7-10 , moves into the category of children about whom you don’t have to worry.
A child who started life with an Apgar score of 5 and remained at the same 5 points 5 minutes after birth ( 5-5 points), needs more careful monitoring. A perfect 10 score is rare.
All indicators are monitored in the first minute after birth, then at the fifth minute of life.
In some cases, especially with low values, the Apgar score is given at the 10th minute of life. Cesarean section babies tend to score higher on the Apgar score because they do not experience difficulty moving through the birth canal.
Mother and relatives are usually told two numbers, for example, 8-9 or 9-9 Apgar scores indicate that the baby’s condition immediately after birth is good.
Here are examples of interpreting Apgar scores
3-3 points- critical condition of the child
5-6 points and below - below average - requires careful monitoring.
6-7, 7-8 scores average - does not require careful observation
8-8 points above average.
8-9, 9-9, 9-10 points - good
10-10 points- perfect (doesn't happen!)
Save on social networks:The Apgar score for newborns is a modern way of assessing the readiness of infants for extrauterine life. The first exam will not affect your love for your baby, but it won’t hurt to learn about the intricacies of passing it and the meaning of the mysterious numbers in the extract from the maternity hospital. Let's talk in more detail about what the Apgar scale is, how to decipher it and what to do if your baby gets low scores.
What does this scale mean?
A scale for assessing the health of a newborn based on external signs is necessary for obstetricians-gynecologists and pediatricians present at the birth. Based on the results of the examination and the summation of points, a decision is made on the mandatory provision of emergency resuscitation care to the baby and on the possibility of transferring him to the mother in labor in a shared ward.
The APGAR system was developed in 1952 as a teaching material for students and an aid in the work of nurses. The innovation was given the name of its creator - an anesthesiologist Virginia Apgar, professor. The invention of the rating was required by the increasing number of cases of births of children with intrauterine pathologies and strangulation during childbirth. And it has been successfully used in obstetrics and pediatrics for 70 years.
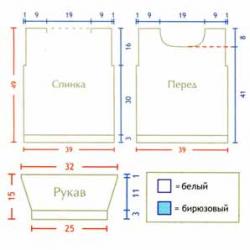
Apgar scale – score range from 0 to 10 points. The child is examined twice in the first and fifth minutes after birth, and scores are assigned according to 5 indicators:
- epidermis color– A (Appearance);
- heart rate– P (Pulse);
- reflexes, reflex excitability– G (Grimace);
- muscle tone, motor activity– A (Activity);
- breathing pattern– R (Respiration).
For each item, the baby receives from 0 to 2 points. After summing up the points, the result on the Apgar scale is ready. If the result of the examination at the fifth minute is 0–7 points, then the assessment is carried out three more times after an equal period of time: at the 10–15–20th minute. Determining the result takes no more than one minute, no additional equipment is required.
In the postpartum discharge, the child has at least 2 indicators on the scale, for example 7/9 or other numbers. This will mean that in the first minute he received 7 points, and in the fifth - 9. To evaluate the result positively, it is important to see the dynamics of adaptation (the first numbers will be less than the subsequent ones).
Learn more about each option
The condition of the newborn is assessed based on external signs of the body’s vital functions. To understand how this happens, let’s look at each point in more detail.






Obstetricians and pediatricians use the table to quickly obtain results on the Apgar scale. She looks like this ( Attention! The table can be scrolled left and right):
| Parameter | 0 points | 1 point | 2 points |
|---|---|---|---|
| Color of the skin | Pale, blue (cyanosis). | The legs and arms are bluish, the rest of the body is pale pink. | The skin tone is even, pink over the entire surface of the body. |
| Heart rate | Single manifestations, no pulse. | Less than 100 beats per minute. | 130–140 beats per minute. |
| Reflexes | Complete absence. | Lack of expression. | Pronounced swallowing, sucking, grasping. |
| Muscle tone | No movement. | Body movements are weak and rare. | Chaotically, regularly swings its limbs. |
| Breath | Absent. | Moans, breathes irregularly (hypoventilation). | Screams, breathes deeply, often. |
The result of the assessment is the summation of points for each indicator. This happens as follows:
- Color of the skin
If a newborn has a light pink or hot pink skin tone, it receives 2 points. A bluish tint to the extremities with a normal color of the epidermis of the rest of the body reduces the score to 1 point and signals the doctor about weak fetal hypoxia.
Everywhere the blue color of the skin, excessive pallor is a reason to carry out resuscitation procedures and give 0 points for the first indicator.
This is interesting! By the way, children born through cesarean section more often receive the maximum 2 points for this criterion. This is due to the fact that the natural passage of the birth canal is not easy for the baby and can affect the level of oxygen in the tissues. But the Caesars manage to avoid this.
- Pulse
Heart rate is measured 6 seconds after birth by auscultation, palpation of the chest or palpation of the arteries. Then they multiply the resulting figure by 10, which gives the minute result.
The heart of newborns works actively. The normal pulse rate is between 130 and 140 beats per minute. In this case, the child earns 2 points.
If the heart beats unstably and slowly, the baby receives 1 point; if there is no pulse at all, 0 points.
If the indicators are not normal, then the baby is given resuscitation procedures until the heart rate returns to normal.
- Reflexes
The ability to suck, grab, swallow, and breathe are the first reflexes of newborns necessary for life. If the child clearly shows the presence of these innate skills in the first minutes of life, then he receives a high score of 2 points. The baby should look for the breast, smack his lips, scream after birth, and breathe.
If reflexes are weakly or partially expressed, then he earns 1 point, if they are completely absent - 0 points.
To obtain an objective assessment, obstetricians stimulate manifestations of reflex movements:
- put a finger to the baby’s lips;
- place the newborn on a flat surface, encouraging him to step;
- lay on the tummy and push under the heels, awakening the crawling reflex;
- a catheter is inserted to clear mucus from the baby’s nose; It’s great if the baby sneezes, grimaces, and moves his head away.
- Muscle tone
Chaotic movements of the arms and legs are the main indicator of the baby’s well-being immediately after birth. He strives to straighten his limbs and bring his body to a normal position. This behavior adds 2 points to the total.
The baby gets 1 point if:
- moves weakly, but does it reluctantly;
- arms and legs remain in a bent position.
With a complete absence of body movements, maintaining the fetal position or close to it - 0 points.
- Breath
The baby earns 2 points if he screams piercingly after birth and in the first minute of life maintains a normal breathing rhythm - 40-45 inhalations and exhalations. If, instead of screaming, the newborn moans, wheezes, or breathes unevenly, he will be given 1 point; if there are no manifestations of this criterion, he will be given 0 points.
Important! It is worth considering that premature babies born unnaturally, but through cesarean section, receive lower Apgar test results. Women should not be upset about this and invent shortcomings for the baby. Attention, care and careful care can quickly correct the situation.
What do ratings mean?

In the delivery room, women are usually not given accurate Apgar scores. Parents see the result in the card after discharge home or find out from the doctor. To decipher the results yourself, use the following decoding of the sum of points.
- 0-2 . The newborn is in a critical situation and requires the help of a resuscitator.
- 3-4 . The indicator is satisfactory. Deviations from the norm are average. Premature babies often get this result. After birth, the baby is observed by a pediatrician, obstetrician, and neurologist.
- 5-6 . Satisfactory result, deviations from the norm are small.
- 7-9 . The indicators are optimally positive. Deviations are weak.
- 10 . Healthy child.
To simplify the algorithm for evaluating the results, we give examples of the results of testing of newborns:
- 8/9, 9/9, 9/10
The baby feels wonderful. Doctors and mother do not need to worry about his well-being and closely monitor his condition until discharge from the hospital.
The clinical result is normal. The baby feels good and has adapted to the external environment quickly.
- 7/8, 6/7, 5/7
Perhaps the baby was born a little weakened, but quickly recovered by the fifth minute. She feels well and does not require medical care or close supervision by a pediatrician.
Satisfactory indicator. Urgent medical attention is not needed.
- 6/6, 5/5
The condition is average; pediatricians need to monitor the newborn more closely.
- 4/5, 5/6
The result is below average, but there is a positive trend. The child is observed more closely for 1–2 weeks after discharge.
- 4/4, 3/4
This result requires measurement at the tenth minute after birth. The baby's physical condition is poor. In this case, the woman and child are placed in a hospital for further observations.
- 2/3, 3/3
Resuscitation is needed, the condition is critical.
- 2/2, 1/2
The child shows obvious signs of asphyxia, and there is a threat to the life of the newborn. Pediatricians must provide immediate resuscitation.
- 0/2, 0/1, 1/1
The situation is difficult, the baby is on the verge of life and death. It is impossible to do without resuscitation and a detailed examination.
This is interesting! A score of 10 is given to newborns in Russia extremely rarely. This is due to the mentality of the medical staff, the fear of jinxing things and showing unprofessionalism. Thus, 9 points can correspond to 10, accepted internationally.
What is considered normal

Newborn Apgar assessment is a worldwide method for detecting defects in intrauterine development of infants. In obstetrics, he was loved for his objectivity and simplicity. The sum of points allows you to get a complete clinical picture of the baby’s condition, draw up a plan for observation and postpartum care for him.
Glasses are considered normal indicators of the level of physical and reflex development from 7 to 10. In this case, the baby does not require medical care; it is handed over to the mother in labor and applied to the breast.
- 5–6 - slight deviations;
Rehabilitation takes time; often the deficiencies are temporary. Associated with asphyxia and fetal immaturity.
- 3–4 - general condition is unsatisfactory;
There is an average degree of oxygen starvation of the baby. Resuscitation procedures will be required to bring breathing and pulse to a normal rhythm.
- 0–2 - critical situation;
There is a risk of death of the newborn. First of all, respiratory stimulation (ventilation) is carried out. The reason for low indicators may be low body weight of the baby, prematurity, hypoxia.
The level of manifestation of the Apgar scale criteria is determined twice: in the first and fifth minutes. When indicators are low, it is important to observe positive dynamics. If a child received 4–5 points in the first minute, but 7–9 in the fifth, then he is considered a healthy child. The lack of dynamics is an alarming sign, a reason to take measurements two or three more times and provide the baby with urgent resuscitation care.
It is important to understand that the Apgar test is subjective for the further development of the baby. Kids with a score of 9–7 will not necessarily be smarter or stronger than those who received low scores.
What if the score is low
Early diagnosis of a newborn’s condition is a lifesaver for modern obstetricians. The Apgar rating indicates the level of well-being of the baby in the first minutes of life. Of course, all parents hope for the birth of a healthy, strong baby, which means high marks on the scale.
Low scores indicate the presence of congenital developmental anomalies and poor adaptation of the infant to the external environment. The most common reasons for negative results are:
- Asphyxia – suffocation. Occurs as a result of entanglement of the fetus with the umbilical cord, obstruction of the respiratory tract with mucus and amniotic fluid.
- Hypoxia is a lack of oxygen during the prenatal period. The brain and tissues do not receive enough oxygen. This results in bluish skin, swelling, and low physical activity in the first minute of life.
- Prematurity. Physiological immaturity, insufficient body weight.
- Birth injury. A healthy fetus suffers during the passage of the birth canal.
- Intrauterine infections. Transmitted from mother to fetus.
- Incompatibility of blood between mother and fetus. Risk of Rh conflict.
Asphyxia and hypoxia are considered especially dangerous. Prolonged lack of oxygen leads to serious developmental problems in the child in the future and provokes serious neurological diseases, such as:
- Syndrome of increased reflex and nervous excitability. It persists in children up to 3 months of age. Babies are restless, often cry, and sleep poorly. Decreased or increased muscle tone, trembling of the chin and limbs are recorded.
- Convulsive syndrome. Leads to epilepsy. Characterized by involuntary contraction of one or a group of muscles.
- Comatose syndrome. Consciousness, sensitivity, and motor function are depressed.
- CNS depression. Reflexes are weak, the baby sleeps a lot and eats little.
- Hydrocephalus. Fluid accumulates in the newborn's brain. A delay in physical and mental development is diagnosed.
Birth trauma causes cerebral palsy, VSD, hypertension, and motor impairment. The consequences of intrauterine infection are difficult to predict. These are various diseases of hearing, vision, internal organs, and stillbirth.
Babies with hypoxia or asphyxia are born weak and passive. The Apgar test result is measured two to four times and is no more than 6 points. By organizing proper care, providing professional medical care, and following pediatricians’ recommendations, normalization of the baby’s condition is possible. And the quality of life of the child and parents will depend on this.
Important! Low Apgar test results in premature babies are similar to average in those born on time unless there is serious cause for concern. For example, 6/7 in immature infants is the norm. But regular observations by a neurologist and other specialized specialists will still be required.
Don't be discouraged if your child's Apgar scores are lower than the maximum. After all, everything that is most important for his development will be laid down further - in the first years of life. And a lot will depend on your love and desire to raise your child healthy and happy.
IMPORTANT! *when copying article materials, be sure to indicate an active link to the original
As soon as the baby is born, he undergoes the first blitz test of independence in his life. Strict examiners are doctors who give scores on the Apgar scale and enter them in the child’s “diary” - an extract for the children's clinic.
At first glance, the test results look quite strange - 6/8, 7/9, 8/9... Let's figure out together what they mean. To do this, you need to understand what this mysterious Apgar scale actually is?
Back in 1952, the famous American anesthesiologist Virginia Apgar developed a special system for assessing the condition of newborns. Each letter in the APGAR test corresponds to a specific body function:
A (appearance) - skin color
P (pulse) - pulse
G (grimace) - grimaces
A (activity) - activity
R (respiration) - breathing
Apgar testing is a system for quickly assessing the condition of a newborn and determining the need for resuscitation measures. The test is a summary analysis of five criteria: skin color, heart rate, reflex excitability, breathing and muscle tone. For each item, the baby is given a score from 0 to 2. Then the results are summed up, and a total score is given from 0 to 10 points.
Evaluation by eye
The baby was born, screamed loudly, and actively worked with its arms and legs - that's a sure 2 points. If he starts to grimace, but breathes unevenly - 1 point. Of course, there are more accurate indicators of the condition of the newborn (for example, oxygen tension in the umbilical cord blood). But to determine this, you need to conduct a special analysis. And the Apgar scale makes it possible to fairly accurately assess the baby’s condition with the naked eye. Moreover, evaluate it in the first minutes of birth, which is very important. Often, help needs to be provided to the baby immediately, and there is simply no time for additional research.
An experienced doctor only needs 40-60 seconds to carry out the test, meaning he can determine the condition of the baby almost at lightning speed. If the baby scores low, he urgently needs medical help. However, test results may vary. To do this, it is carried out at least twice - at the 1st and 5th minutes after birth (hence the double score: for example, at the first minute 6, at the second 9, it turns out 6/9). It often happens that in the 1st minute the baby receives a very low score. But after resuscitation procedures, he gains the necessary points. The baby just needed time and help to adapt to new, unusual conditions. If during the second test, that is, at the 5th minute, the Apgar score is less than 7 points, the baby will be tested again every 5 minutes for the next 20 minutes and at the same time the necessary procedures will be carried out.
Apgar score: what are we testing?
Rating "Excellent"
10-9 points - the baby is healthy, all body systems are activated on time, and the newborn does not need medical attention.
Rating "Good"
8-7 points - the baby passed the exam, the doctors have no special reasons for worry (the baby suffered acute oxygen starvation, but then his condition stabilized).
Rating "Satisfactory"
6-5 - the situation is not very good, the baby will most likely be placed in the pediatric intensive care unit under the supervision of nurses. Here they will monitor the vital functions of the body. The baby will be brought to the mother when all body systems begin to work stably.
Rating "Poor"
4-0 points - the newborn needs emergency care, resuscitation measures must be taken urgently (since there is a danger to the child’s life).
| 0 points | 1 point | 2 points | |
| Color of the skin | Excessive pallor or blueness | Body pink, limbs bluish | Pink body and limbs |
| Number of cardiovascular contractions | No heartbeat | Less than 100 heartbeats in 2 minutes | 100 or more heartbeats per minute |
| Reflex excitability (reaction to mucus pumping out) | No reaction | Displeased grimace, weak movements | Coughing, sneezing, loud screaming |
| Muscle tone | Absent, body relaxed, limbs hanging | The tone is reduced, the limbs bend | Facial expression: curled up into a ball, arms and legs bent |
| Presence of spontaneous breathing | Not breathing | Irregular single breaths, weak cry | Normal breathing, loud scream |
Excellent and good students
Only 15% of newborns receive 10 points in the first minute. Most babies need some time for all body systems to work at full capacity outside the mother's body.
Borderline score: 7 points. In this case, a lot depends on the professionalism of the doctors and on how the baby adapts to new conditions. The first assessment indicates the amount of necessary assistance that needs to be provided to the baby. But this is in no way an indicator of the baby’s further development. But the second assessment can already predict health problems. Therefore, if the second score is low, the baby will be observed by a neurologist for the first year of life. The lower the second score, the higher the likelihood of damage to the central nervous system. As a rule, a low score is due to the fact that the baby experienced oxygen starvation, that is, was in a state of hypoxia (chronic hypoxia - oxygen starvation during pregnancy and acute hypoxia - oxygen starvation during childbirth). Premature babies often have lower scores than those born on time.
The Apgar scale makes it possible to fairly accurately assess the baby’s condition with the naked eye, and in the first minutes of birth.
Calm, just calm!
Apgar scores are included in the statement for the children's clinic, which is handed out to them. Many parents are frightened when they see that their child did not immediately become an "excellent student" and his grade is too low. Remember, it has nothing to do with the child’s intellectual potential, but only determines the baby’s condition right away. Parents' fears are sometimes excessive. Yes, such a baby will need more attention, you may have to take more massage courses and do therapeutic exercises with him. But it's not that difficult! Recent research by doctors confirms that most of these babies grow up quite healthy. In recent years, there has been a lot of controversy about how objective the Apgar system is. Thus, psychologists say that every baby has its own character and temperament from birth. Obviously, a baby who is more passive from birth will not actively move or scream loudly, and this does not mean at all that he is sick. Future quiet people will most likely just whine and quickly calm down. And the bullies and daredevils will scream loudly as soon as they are born. By the way, Virginia Apgar herself also called her system rather conditional. So it is premature to panic because of low indicators.
Apgar scores, along with height and weight, are the first and most significant in your baby’s life. During the first year of the baby's life, doctors will ask the mother what Apgar score he was born with. So memorize these two numbers and don’t forget: no matter who your baby is - an excellent student or a C student - he really needs your care and love. There are never too many of them.
Comment on the article "First exam: Apgar score"
Thank you! Very good article - everything on the shelves. I have never come across such detailed information about the APGAR assessment. My first child was born 4/6 points - he almost suffocated during childbirth. When our pediatrician saw this assessment, she immediately asked why he was not breathing, and for a long time I wondered how she immediately realized that the low score was precisely because of breathing.
Total 1 message .
More on the topic "Good assessment of the condition of the newborn using the Apgar scale":
The child does not have information about the Apgar school in his medical record. Is this very important to know when deciding to adopt?
Why, apparently I’m completely dark... I read in reports all the time about this mythical Apgar.... girls, tell me what this means?
First exam: Apgar score. Lekha was given 8/9. I later compared it with the table, and it clearly wasn’t more than 7... the Apgar scale. Care and education of a child up to one year: nutrition, illness, development. Apgar scale. Girls, who had what scores? interesting and...
First exam: Apgar score. Obviously, a baby who is more passive from birth will not actively move or scream loudly, and this does not mean at all that he is sick. So memorize these two numbers and don't forget: whoever your baby is...
First exam: Apgar score. Only 15% of newborns receive 10 points in the first minute. Most babies need some time for all body systems to work at full capacity outside the mother's body. Borderline score - 7 points.
First exam: Apgar score. Back in 1952, the famous American anesthesiologist Virginia Apgar developed a special one. Each of the letters of the APGAR test corresponds to a specific body function.
Girls, who had what scores? I wonder if they give it 10/10
Apgar scale - assessment of the newborn's condition, good Apgar score. How are points calculated? Since then, the health of the newborn is assessed based on five indicators: breathing, heartbeat, muscle tone, reflexes and skin color.
Well, almost everyone here knows that I’m a fool. Girls, help. I read a discussion that asphyxia and hypoxia during childbirth affect developmental delays, autism, etc. Our Apgar score was 7-8, he started screaming right away. The pack says 8-10 is normal, 5-6 is moderate hypoxia, 1-4 is severe. Is seven normal or is it hypoxia? What are your Apgar scores?
First exam: Apgar score. What is an "Apgar score"? Print version. 4.4 5 (43 ratings) Rate this article. Each letter in the APGAR test corresponds to a specific bodily function.
what does it mean?
Examination of the child’s condition using the Apgar scale: frequency is checked. The condition of the newborn is assessed as “good” if 8-10 points are satisfactory. This is only an assessment of the NEWBORN's condition. Sometimes the reanimated children in the future will show...
Mommies! What Apgar scores were you given? I want to compare them with ours
Is 5 on the Apgar scale very bad? My friend just had an emergency caesarean section, we are worried. Has anyone had that many?
I wonder if anyone gets an Apgar score of 10/10? Or do our maternity hospitals never see such healthy children? And also, is this assessment announced immediately or do you have to ask yourself later?
Unfortunately, this birth did not go very well for us. The child had asphyxia, Apgar score 5/7. The umbilical cord turned out to be too short and tight on the neck, there were difficulties. It's interesting to talk to those who have had something similar. What did the doctors tell you about the consequences, where did they look, etc.? How do your children develop, are there any predicted consequences, how do you deal with them?
Girls, please explain in more detail what a 10 Apgar score is!
Apgar score. I Heart rate: no pulse --- 0 Slowing (less than 100 per 1 min) 1 More than 100 per 1 min 2 II Respiratory movements Absent 0 Rare, irregular 1 Apgar scale - assessment of the condition of the newborn, good score on the Apgar scale.
The point system at school is a clear scheme for assessing knowledge according to certain criteria. If we talk about the Apgar score - a system for assessing the health of a newborn, then it is subjective. Compared to school, there is not a wide range of grades. The midwife does them by eye during examination.
In order for future mothers to understand exactly how the condition of their child will be assessed after childbirth, we will consider in detail the principle of this scale itself.
How the scale works
What is the Apgar scale and who is its founder? Virginia Apgar, a famous American professor of anesthesiology, introduced a scale for assessing the health status of a newborn child back in the 50s of the last century. The main goal of her method was to promptly identify babies in need of resuscitation measures. Initially, the scale was intended for nursing staff. It was used to determine which child needed more attention.
The technique was named after its founder. Sixty years of experience in using such assessment of a newborn gives reason to believe that the Apgar scale is still quite simple and reliable for a comprehensive assessment. According to many experts, it is a little subjective, because points are given only on the basis of an obstetric examination of the child. The rating scale ranges from 0 to 2 points, where 0 is given for the absence of a certain feature, 1 is given for its average severity, 2 for a well-expressed feature.
Let's look at what exactly is assessed on the scale. It should be noted that for ease of assessment, the English transcription of Mrs. Virginia’s surname was taken. In the word APGAR, each letter stands for a specific evaluation parameter.
- A - activity - activity and muscle tone of the child. A healthy baby has arms and legs pressed to the body, fists clenched. The child is active, moves, his face expresses emotions of peace or dissatisfaction with a cry.
- P - pulse - pulse. The baby's heart rate is normally 130-140 beats per minute. If this indicator in a newborn is more than one hundred beats per minute, then it is given 2 points, less than one hundred - 1 point, and the absence of heart rate is recorded as 0 points.
- G - grimace response - the child’s grimaces, the manifestation and degree of expression of the newborn’s unconditioned reflexes.
- A - appearance - skin color and appearance of the child. Shades of pink (from bright to pale) are considered normal. The presence of blueness of the skin, called cyanosis, provides grounds for reducing the score.
- R - respiration - the child’s cry, his breathing, reflex excitability. If a newborn screamed loudly and piercingly immediately after birth, then the score for this parameter is 2 points. A weak cry turning into a squeak, low breathing rate is assessed as 1 point. Lack of breathing and screaming - 0 points.
Assessment results and forecasts
The Apgar scale is used twice to assess the condition of a newborn: in the first and fifth minutes of his life. The first minute assessment shows how the baby experienced the birth. The second assessment indicates the degree of its adaptation to the environment.
Condition results are recorded as a fraction, where the first number represents the first assessment and the second number represents the assessment during the second measurement. It should be emphasized that this scale is not the basis for making further forecasts of the child’s condition and health.
Its results are interpreted as follows:
- 7-10 points - no deviations in health status were identified;
- 5-6 points - minor deviations;
- 3-4 points - significant deviations from the norm;
- 0-2 points - threat to the life of the newborn.
Children with the best results are considered to be in excellent condition and require only routine care. A score of up to 6 points indicates a satisfactory condition and the need for some resuscitation procedures. A child with a score of less than 4 points requires such procedures immediately. If the sum during the second measurement is less than 7, then additional measurements must be taken every 5 minutes. A child who receives 5-6 points on the first measurement and 7-10 on the second goes into the category of healthy children. It should be noted that an Apgar score of 10 is quite rare.
Let us remind you once again about the subjectivity of the Apgar scale and that it is not a method for predicting the development of a baby. Therefore, it cannot be said that a child with a 9-point score will be smarter or healthier than one who received 6 points. The development, health, and abilities of each child are directly proportional to the care, love, and attention of his parents.
Especially for Elena TOLOCHIK
Every modern mother in labor knows that when recording the parameters of a born child, weight, height and the newborn’s Apgar score are used.
If everything is clear with the measurements of height and weight, then by what criteria is the mysterious assessment given?
An anesthesiologist from America, Virginia Apgar, has developed a special table to help her resuscitation students, which allows them to clearly determine the condition and viability of the baby in the first minutes of a child’s birth.
The purpose of the scale is to quickly assess the condition of a newborn child regarding the need for resuscitation measures.
What indicators are assessed?
The condition of the newborn on the Apgar scale is assessed according to five main criteria:
- Coloring of the skin of the body and limbs.
0 - Pale bluish color of the body and limbs.
1 - Partially bluish color of the limbs.
2 - Healthy pink color throughout the body.
- Heart rate per minute.
0 - Not present.
1 - Up to 100 beats per minute.
2 - 100 or more beats per minute.
- Reflexes.
0 - Does not respond.
1 - Weak reaction, sluggish movements, grimace on the face.
2 - Moves actively, coughs, sneezes, screams.
- Muscle tone.
0 - Absent, limbs hanging down.
1 - The tone is reduced, weak movements of the arms and legs are observed.
2 - The tone of the limbs is actively expressed, vigorously moves the arms and legs.
- Breath.
0 - Not breathing.
1 - Shallow, irregular breathing, weak cry, slow breathing.
2 - Breathes normally, screams loudly.
For each criterion, the obstetrician and neonatologist give the child 0, 1 or 2 points. The final figure is the sum of points for all parameters of the Apgar table.
The child's condition is assessed using the Apgar scale in the 1st minute after the birth of the fetus. The second point is the same parameters assessed at the 5th minute.
Sometimes, with very low indicators, doctors give a third estimate at the 10th minute of the newborn’s independent life. Parents are usually given a double score, for example 7/9.
A score of 3 or less on the scale indicates an unfavorable condition of the child and the need for special life support measures.
7 points and above – the child is normal, viable, and has a good chance of gradually adapting to independent life.
Decoding the Apgar scale
Assessing the condition of the newborn helps doctors, if necessary, quickly take measures to support the child’s life:
- From 0 to 2 points.
The child's viability is at risk. Immediate resuscitation measures are required.
When timely professional assistance is provided, the baby shows the best Apgar result 5 and 10 minutes after birth.
Subsequently, the baby will need more careful care and monitoring. However, it is believed that even “B” students are capable of becoming physically strong and smart children in the future.
This is how premature babies are usually assessed. If the condition does not improve in the 5th minute, resuscitation is required, as well as special attention and care in the first weeks of life.
The condition of the newborn is considered satisfactory. The baby will need close medical supervision in the first week of life.
If the condition at the 5th minute of life has improved to 7-8 points on the Apgar scale, then a stay in intensive care is not required.
Optimized assessment of child viability. The baby tolerated the birth well and is not at risk. Doctors only make sure that the process of feeding and weight gain improves.
If the mother has enough milk and the baby is gaining weight, then his condition is not in danger.
- 10 points.
Highest Apgar score. During natural childbirth, the child rarely receives the highest score in all respects.
An Apgar score of 9/9 is considered excellent. Russian doctors do not give 10 simply so as not to jinx it. In the reports of foreign obstetricians, you can often find the number 10.
It is believed that “caesareans”, under equal pregnancy conditions, may have a higher Apgar score, since they did not have to endure the stress associated with passing through the birth canal.
In 1963, pediatrician Joseph Butterfield used the letters of Virginia Apgar's surname as an abbreviation to better memorize the table of Apgar scores.
This mnemonic rule helps English-speaking specialists keep in mind all the columns of the Apgar table:
- A ppearance – appearance.
- P ulse – heart rate
- G rimace – facial expression, reflexes.
- A ctivity - movement.
- R espiration – respiratory activity.
Acronyms of the same nature also exist among specialists in the German and Spanish language environment.
In American English, a neologism has appeared that deciphers the abbreviation APGAR - American Pediatric Gross Assessment Record (General American Pediatric Gross Assessment Record). We are, of course, talking about the newborn assessment system, famous among obstetrics all over the world.
In the English-speaking environment, there is also another principle of simplified memorization of Apgar scale data - H ow R eady I s T he C hild (how prepared the child is)
- H heart rate – heart rate.
- R espiratiry effort - respiratory activity.
- I rritability is a reflex response to stimuli.
- T one – muscle tone.
- C olor – color of the skin.
Why doesn’t a healthy baby with an easy birth get an Apgar score of 10?
Each child individually experiences the process of adaptation to independent life outside the mother’s body. Assessing viability using this table is considered objective, but there are also subjective factors:
- In order for the baby’s circulatory system to fully function on its own, it takes about 5 minutes. Until this time has elapsed, the arms and legs may retain a bluish coloration.
- There are cases when a healthy baby receives a low Apgar score only because he does not scream, but with interest and carefully examines the new environment in which he finds himself.
- The professionalism of the doctor also influences the analysis of the situation in the first minutes after childbirth. This is just a kind of test for the physiological criteria of the baby’s viability.
Decoding the Apgar score does not affect the physical development and intellectual usefulness of the child.
In the first year of life, scores at birth of a child of 8/8 or other possible combinations of scores will be of interest to the pediatrician, pediatric neurologist and other highly specialized pediatric doctors.
Read also: